Note: The following article is heavily influenced by my training from Functional Movement Systems (FMS). For more information, I recommend the SFMA Levels I and II courses.
When many people go to their doctor for knee pain, their doctor may run through a battery of tests to assess the state of the knee joint. X-rays, MRIs, and various orthopedic diagnostics may be employed in hopes of finding the source of the problem.
How often, however, are doctors also examining the ankle and hip mobility of their knee-pain patients? In many cases, pain in areas such as the knee or low back are often influenced by a lack of mobility at nearby joints, and range of motion assessment could be a key diagnostic for uncovering the source of pain.
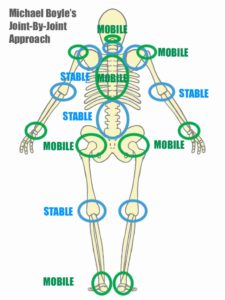
The Joint-By-Joint Approach
According to the “Joint-By-Joint” Approach, the human body is essentially a stack of sable segments sitting on top of mobile joints. Some joints tend to require more mobility, while other joints tend to require more stability, and in general, the stability/mobility demands of each joint tend to alternate as seen below:
When we are lacking range of motion at one of the mobile joints, the body has no choice but to compensate and create extra motion at one of the stable joints.
For example, somebody lacking hip flexion may compensate by creating excessive flexion at the lumbar spine. Somebody lacking shoulder motion may compensate by creating excessive scapular elevation or anterior tilt. Somebody lacking ankle dorsiflexion may overly pronate and collapse the knee into valgus during gait.
Over time, this can put unfavorably high amounts of stress and load on the compensating joints and lead to injury or pain.
Research Examples
- Lack of hip range of motion is a risk factor for low back pain (1-16)
- Lack of hip range of motion is a risk factor for knee pain (17-19)
- Lack of ankle dorsiflexion can increase likelihood of knee valgus and is a risk factor for knee pain (20-26)
- Lack of shoulder range of motion is a risk factor for elbow pain (27-28)
Conclusions
For these reasons, it is not hard to see why maintaining proper joint mobility is essential for injury prevention. When mobility is lacking, joint compensations occur, and over time these compensations can be a major contributor to pain or injury.
References
- Barbee-Ellison JB, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: comparisons between healthy subjects and patients with low back pain. Phys Ther 1990;70:537 – 41.
- Burns SA, Mintken PE, Austin GP. Clinical decision making in a patient with secondary hip-spine syndrome. Physiother Theory Pract. 2011;27(5):384-397.
- Chesworth BM, Padfield BJ, Helewa A, et al. A comparison of hip mobility in patients with low back pain and matched healthy subjects. Physiotherapy Canada. 1994; 46: 267-74.
- Chesworth BM, Padfield BJ, Helewa A, et al. A comparison of hip mobility in patients with nonspecific low back pain. Physiother Can 1994;46:267–74
- Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. 1998; 23: 1009-1015.
- Devin CJ, McCullough KA, Morris BJ, Yates AJ, Kang JD. Hip-spine syndrome. J Am Acad Orthop Surg. 2012;20(7):434-442.
- Ellison, JB, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Phys Ther. 1990; 70(9): 537-541.
- Harris-Hayes, M., Sahrmann, S. A., & Van Dillen, L. R. (2009). Relationship between the hip and low back pain in athletes who participate in rotation-related sports. Journal of sport rehabilitation, 18(1), 60-75.
- Kujala, U. M., Taimela, S., Salminen, J. J., & Oksanen, A. (1994). Baseline anthropometry, flexibility and strength characteristics and future low‐back pain in adolescent athletes and nonathletes. Scandinavian journal of medicine & science in sports, 4(3), 200-205.
- Mellin G. Correlation of hip mobility with degree of back pain and lumbar spinal mobility in chronic low back pain patients. Spine. 1988; 13: 668-670.
- Prather, H., Cheng, A., Steger-May, K., Maheshwari, V., & Van Dillen, L. (2017). Hip and Lumbar Spine Physical Examination Findings in People Presenting With Low Back Pain, With or Without Lower Extremity Pain. journal of orthopaedic & sports physical therapy, 47(3), 163-172.
- Reiman MP, Weisbach PC, Glynn PE. The hips influence on low back pain: a distal link to a proximal problem. J Sport Rehabil. 2009;18(1):24-32.
- Roach, S. M., San Juan, J. G., Suprak, D. N., Lyda, M., Bies, A. J., & Boydston, C. R. (2015). Passive hip range of motion is reduced in active subjects with chronic low back pain compared to controls. International journal of sports physical therapy, 10(1), 13.
- Vad VB, Bhat AL, Basrai D, et al. Low back pain in professional golfers: the role of associated hip and low back range of motion deficits. Am J Sports Med. 2004; 32(2): 494-497.
- Van Dillen LR, Bloom NJ, Gombatto SP, Susco TM. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008 May;9(2):72-81.
- Van Dillen, L. R., Sahrmann, S. A., Norton, B. J., Caldwell, C. A., Fleming, D., McDonnell, M. K., & Bloom, N. J. (2001). Effect of active limb movements on symptoms in patients with low back pain. Journal of Orthopaedic & Sports Physical Therapy, 31(8), 402-418.
- Cliborne AV, Wainner RS, Rhon DI, et al. Clinical hip tests and a functional squat test in patients with knee osteoarthritis: reliability, prevalence of positive test fi ndings, and short-term response to hip mobilization. J Orthop Sports Phys. Ther. 2004;34(11):676-685.
- Currier LL, Froehlich PJ, Carow SD, et al. Development of a clinical prediction rule to identify patients with knee pain and clinical evidence of knee osteoarthritis who demonstrate a favorable short-term response to hip mobilization. Phys Ther. 2007;87(9):1106 1119.
- VandenBerg C, Crawford EA, Sibilsky Enselman E, Robbins CB, Wojtys EM, Bedi A. Restricted Hip Rotation Is Correlated With an Increased Risk for Anterior Cruciate Ligament Injury. Arthroscopy. November 2016. doi:10.1016/j.arthro.2016.08.014.
- Backman, L. J., & Danielson, P. (2011). Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study. The American journal of sports medicine, 39(12), 2626-2633.
- Bell-Jenje, T., Olivier, B., Wood, W., Rogers, S., Green, A., & McKinon, W. (2016). The association between loss of ankle dorsiflexion range of movement, and hip adduction and internal rotation during a step down test. Manual therapy, 21, 256-261.
- Dill, K. E., Begalle, R. L., Frank, B. S., Zinder, S. M., & Padua, D. A. (2014). Altered knee and ankle kinematics during squatting in those with limited weight-bearing–lunge ankle-dorsiflexion range of motion. Journal of athletic training, 49(6), 723-732.
- Fong CM, Blackburn JT, Norcross MF, McGrath M, Padua DA. Ankle-dorsiflexion range of motion and landing biomechanics. J Athl Train. 2011;46(1):5–10.
- Macrum, E., Bell, D. R., Boling, M., Lewek, M., & Padua, D. (2012). Effect of limiting ankle-dorsiflexion range of motion on lower extremity kinematics and muscle-activation patterns during a squat. Journal of sport rehabilitation, 21(2), 144-150.
- Rabin, A., Portnoy, S., & Kozol, Z. (2016). The Association of Ankle Dorsiflexion Range of Motion With Hip and Knee Kinematics During the Lateral Step-down Test. journal of orthopaedic & sports physical therapy, 46(11), 1002-1009.
- Vesci BJ, Padua DA, Bell DR, Strickland LJ, Guskiewicz KM. (2007). Influence of hip muscle strength, flexibility of hip and ankle musculature, and hip muscle activation on dynamic knee valgus motion during a double-legged squat. J Athl Train;42(2 Suppl):S-83.
- Garrison, J. C., Cole, M. A., Conway, J. E., Macko, M. J., Thigpen, C., & Shanley, E. (2012). Shoulder range of motion deficits in baseball players with an ulnar collateral ligament tear. The American journal of sports medicine, 40(11), 2597-2603.
- Wilk, K. E., Macrina, L. C., Fleisig, G. S., Aune, K. T., Porterfield, R. A., Harker, P., … & Andrews, J. R. (2014). Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. The American journal of sports medicine, 42(9), 2075-2081.